Hyperventilation Strategies for Optimized ANEclear Performance
Joseph Orr, PhD – Research Professor University of Utah Department of Anesthesiology
 Tidal volume (the volume of each breath) can be inadvertently reduced when the respiration rate is increased during emergence.
Tidal volume (the volume of each breath) can be inadvertently reduced when the respiration rate is increased during emergence.- Increasing the inspiratory flow rate and or the inspiratory pressure limit will usually prevent tidal volume reduction.
- Be sure to observe the measured tidal volume during emergence. If you are not sure where the measured tidal volume is displayed, watch the movement of the anesthesia machine bellows.
Successful application of ANEclear requires hyperventilation during emergence. Hyperventilation means substantially higher ventilation than the patient received during the maintenance period of the anesthetic. For example, if minute volume during maintenance was 5 L/min, we would expect 10-15 L/minute during emergence. However, hyperventilation achieved with high respiration rates and small tidal volumes is not productive; tidal volume must be maintained during emergence for successful outcomes. Adequate tidal volume is required for ANEclear performance and safety. The labeling requires a minimum of at least 500 ml. The ideal volume is equal to the patient’s own anatomic dead space, plus the dead space added by the other apparatus in the breathing circuit (filter, sampling adaptor etc.) and the dead space of ANEclear . This means that tidal volumes of between 700 and 1000 ml are ideal. Very large tidal volumes are not indicated in some patients. Remember, if the patient cannot safely tolerate tidal volumes of at least 500 ml during emergence, ANEclear should not be used.
While no one has intentionally delivered small tidal volumes during emergence with ANEclear , some users inadvertently set the ventilator in ways that lead to smaller tidal volumes during emergence. An all too common scenario occurs when the set respiration rate is increased during emergence and the delivered tidal volume decreases such that Minute Ventilation actually falls.
There are two main reasons why the tidal volume can shrink when the respiratory rate increases: inadequate inspiratory flow rate and exceeding the pressure limit. Inadequate flow rate is corrected by simply increasing the set inspiratory flow rate. Pressure limit problems are usually resolved by increasing the set pressure limit. It is often the case that both the inspiratory flow rate and the pressure limit are left at whatever setting was used during the previous case and no attention is given to either setting. Re-adjusting these settings prior to emergence will help ensure adequate ventilation during emergence leading to rapid emergence when using ANEclear.
Inadequate Inspiratory Flow Problem
The inspiratory flow rate determines the rate at which the ventilator delivers gas to the lungs. If the set respiratory rate is low, there is plenty of time for complete tidal volume to be delivered even if the inspiratory flow rate is low. However, if the respiratory rate is increased, then the time allowed for the ventilator to push gas into the lungs is reduced, and there may not be enough time for the complete volume to be delivered. The simple solution is to increase the inspiratory flow rate. By increasing the inspiratory flow rate, then the ventilator can still deliver the set tidal volume even though the time allotted to each inspiration has been reduced.

Pressure Limit Problem
During inspiration, the ventilator pushes gas into the lungs. As the volume of gas in the lungs rises, the pressure required to push the gas rises as well. Because excessive pressure can damage the lungs, the ventilator will stop delivering gas once the pressure exceeds a set limit. This“peak pressure limit” is an adjustable setting on the ventilator that is built into the anesthesia machine. Once the pressure measured by the ventilator reaches the set pressure limit, then gas delivery stops and the delivered tidal volume is only the amount of gas that was delivered before the pressure limit was reached. The problem we face is that the pressure that is measured by the ventilator as it pushes gas toward the lungs is not the same as the actual pressure in the lungs. The pressure that the ventilator sees is the pressure in the lungs plus all of the back pressure required to push gas through additional devices placed in the path between the ventilator and the lungs. These devices include the endotracheal tube, the bacterial/viral filter, ANEclear, the breathing circuit hose, the anesthesia machine check valve, etc. The amount of back pressure is small when the gas flow rate is low. This is often the case when the respiration rate is low. But when the gas flow rate is increased, the added back pressure caused by pushing gas rapidly through the breathing circuit rises. In some cases, doubling the inspiratory flow rate can raise the back pressure fourfold.
On some newer electronic ventilators, raising the respiration rate tells the ventilator to automatically raise the flow rate during inspiration. This means that when you double the respiration rate, you tell the ventilator to double the gas flow rate during inspiration. This causes the back pressure to rise causing the pressure to exceed the limit and therefore causing the delivered tidal volume to drop.
As an example, consider a situation in which the respiration rate is set at 10 breaths per minute during maintenance and the added back pressure during each inspiration is 8 cm H2O. If the breath rate is increased to 20 breaths per minute during emergence, then the back pressure might increase from 8 to 32 cm. H2O. Adding 32 cm H2O of back pressure to the actual pressure in the lungs of about 15 cm H2O will exceed a normal peak pressure limit set at 30 cm H2O and therefore only a small volume will be delivered to the lungs.
The simple solution to this problem is to simply raise the set peak pressure limit on the ventilator. This will allow the full tidal volume to be delivered regardless of the back pressure induced by increased flow rate. Note that on some machines, the high pressure limit is set by adjusting an alarm limit. This means that adjusting the high pressure alarm limit automatically adjusts the maximum pressure that the ventilator will deliver.
The peak inspiratory pressure limit is provided as a safety mechanism to prevent “barotraumas” or damage to the lungs due to over-inflation. Most clinicians understand that the actual pressure in the lungs is much less than the pressure seen by their ventilator and displayed on their monitor screens and that increasing the pressure limit does not mean that the lungs will experience the set pressure limit. However, there is a limit beyond which the pressure limit can not be increased.
If the pressure limit is already at the maximum safe level, an alternative approach is to increase the time allotted to inspiration during each breath by adjusting the I:E ratio setting on the ventilator. The I:E ratio is the ratio of inspiration time relative to expiration time for each breath. For example, if the I:E ratio is set at 1:3, then for every one second of inspiration time, there will be three seconds of expiration. Decreasing the I:E ratio gives more time for inspiration and therefore lowers the flow rate needed to deliver the set tidal volume. Lower flow rates mean less back pressure so more volume can be delivered to the lungs without reaching the peak pressure limit.
As an example, consider a case in which the set respiration rate is 10 breaths per minute and the I:E ratio is 1:3 during maintenance. This means that inspiration lasts 1.5 seconds and expiration lasts for 4.5 seconds for each breath. If the breath rate is doubled during emergence, then the time allowed for each inspiration drops to 0.75 seconds, and the ventilator would need to double the flow rate to deliver the entire breath in the shortened time. The doubled flow rate will cause an increase in back pressure causing the peak pressure limit to be reached and the tidal volume to be decreased. If the I:E ratio is adjusted lower, to 1:1, then the time allowed for inspiration remains at 1.5 seconds and the ventilator does not have to increase flow rate even though the respiration rate has doubled. In this manner, the respiratory rate can be doubled and the peak pressure does not increase.
Another method of raising the delivered volume is to increase the respiratory rate less dramatically. For example, doubling the respiration rate, without changing the I:E ratio might cause a fourfold increase in back pressure; however, a 50% increase in respiration rate might only raise the back pressure twofold. This means that if respiratory rate is high and tidal volume has fallen, it may be wise to decrease the respiration rate until the tidal volume has been restored to its set value. One strategy is to decrease the respiratory rate in small steps (1-2 breaths per minute) until the set tidal volume is delivered.
So the first strategy is to increase the peak pressure limit. If the pressure limit is already at the highest safe level, then adjust the I:E ratio down. Both of these adjustments can be done prior to emergence. If neither of these strategies is available, decrease respiration rate in steps of 1-2 breaths/minute until the set tidal volume is achieved.
MONITORING ISSUES
Two Tidal Volumes
Electronic anesthesia machines display two versions of tidal volume. One is the set tidal volume selected by the user; the other is measured tidal volume. The measured tidal volume is the volume of exhaled gas for the most recent breath. When there is a problem with the inspiratory flow rate or the pressure limit, the measured tidal volume will be less than the set volume.
Watch The Bellows
 If you cannot see, or cannot locate, the measured tidal volume display on the anesthesia machine screen, watch the bellows. The bellows rise and fall with each breath. There are marks on the side of the bellows showing the volume corresponding to the position of the bellows. If the rise and fall of the anesthesia machine bellows is not approximately equal to the set tidal volume, then the set tidal volume is not being delivered. If the movement of the bellows does not indicate at least 500 ml volume during emergence, ANEclear will not give the rapid emergence that is expected.
If you cannot see, or cannot locate, the measured tidal volume display on the anesthesia machine screen, watch the bellows. The bellows rise and fall with each breath. There are marks on the side of the bellows showing the volume corresponding to the position of the bellows. If the rise and fall of the anesthesia machine bellows is not approximately equal to the set tidal volume, then the set tidal volume is not being delivered. If the movement of the bellows does not indicate at least 500 ml volume during emergence, ANEclear will not give the rapid emergence that is expected.
Minute Volume Delay
Remember that “tidal volume” is the volume of gas delivered during each breath, “respiration rate” is the number of breaths delivered each minute and “minute volume” is the total volume of the breaths delivered in the past minute. Since the minute volume is the sum of breaths given in the past minute, it will not reflect changes in tidal volume and or respiration rate until nearly a minute later. That is why the displayed minute volume often does not equal tidal volume multiplied by respiration rate. This delay between when adjustments are made and when the displayed minute volume is correct can lead to errors in ventilator adjustment.
A DRY RUN
If safe and practical, hyperventilate the patient during the maintenance phase of the anesthetic. Test your strategy for 2-3 minutes during the time when there is not much for the anesthesiologist/ CRNA to do during the surgery. Remember that it will take at least 1 minute to observe the complete effect of any setting change on the displayed minute volume. In any case they can quickly see that the tidal volume does not change when respiration rate in increased. This will give them a chance to test their settings for pressure
limit, I:E ratio etc. and be sure that all is as it should be prior to emergence
DEMONSTRATION CASE
The photo below was taken at a demonstration at a University located in the south eastern area of the United States. The set tidal volume was 875 ml. and the measured tidal volume was much less, only 156 ml. The machine showed warning messages saying that the set tidal volume was not delivered and that the peak pressure was high, but neither were noticed. The displayed minute volume was 9.4 liters, while the actual, instantaneous minute volume was only 3.9 liters. The displayed minute volume is left over from the minute before emergence when the tidal volume was still large. The peak pressure was 42 cm H2O which was in excess of the pressure limit setting which was most likely set at 40 cm H2O. The I:E ratio was set at 1:2.
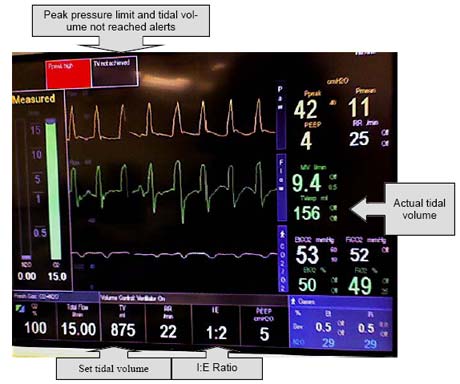
In this case, the emergence was slower than expected. The set tidal volume was large and the delivered tidal volume was sufficient prior to emergence when the respiratory rate was 11 breaths per minute. When the respiratory rate was increased to 22, the pressure limit was reached during inspiration and the tidal volume dropped. In this case, the minute volume during emergence was less than half the maintenance minute volume. Because the small tidal volume was about the same as the patient’s dead volume (volume in the trachea that does not participate in gas exchange) there was virtually no gas exchange in the lungs. Had this problem been recognized, any of the three strategies suggested earlier could have corrected this situation. Either raising the peak pressure limit, adjusting the I:E ratio to 1:1 or stepping down the respiration rate would have caused higher tidal volumes and a faster emergence.
Hyperventilation Strategies for Optimized ANEclear Performance
Joseph Orr, PhD – Research Professor University of Utah Department of Anesthesiology

- Tidal volume (the volume of each breath) can be inadvertently reduced when the respiration rate is increased during emergence.
- Increasing the inspiratory flow rate and or the inspiratory pressure limit will usually prevent tidal volume reduction.
- Be sure to observe the measured tidal volume during emergence. If you are not sure where the measured tidal volume is displayed, watch the movement of the anesthesia machine bellows.
Successful application of ANEclear requires hyperventilation during emergence. Hyperventilation means substantially higher ventilation than the patient received during the maintenance period of the anesthetic. For example, if minute volume during maintenance was 5 L/min, we would expect 10-15 L/minute during emergence. However, hyperventilation achieved with high respiration rates and small tidal volumes is not productive; tidal volume must be maintained during emergence for successful outcomes. Adequate tidal volume is required for ANEclear performance and safety. The labeling requires a minimum of at least 500 ml. The ideal volume is equal to the patient’s own anatomic dead space, plus the dead space added by the other apparatus in the breathing circuit (filter, sampling adaptor etc.) and the dead space of ANEclear . This means that tidal volumes of between 700 and 1000 ml are ideal. Very large tidal volumes are not indicated in some patients. Remember, if the patient cannot safely tolerate tidal volumes of at least 500 ml during emergence, ANEclear should not be used.
While no one has intentionally delivered small tidal volumes during emergence with ANEclear , some users inadvertently set the ventilator in ways that lead to smaller tidal volumes during emergence. An all too common scenario occurs when the set respiration rate is increased during emergence and the delivered tidal volume decreases such that Minute Ventilation actually falls.
There are two main reasons why the tidal volume can shrink when the respiratory rate increases: inadequate inspiratory flow rate and exceeding the pressure limit. Inadequate flow rate is corrected by simply increasing the set inspiratory flow rate. Pressure limit problems are usually resolved by increasing the set pressure limit. It is often the case that both the inspiratory flow rate and the pressure limit are left at whatever setting was used during the previous case and no attention is given to either setting. Re-adjusting these settings prior to emergence will help ensure adequate ventilation during emergence leading to rapid emergence when using ANEclear.
Inadequate Inspiratory Flow Problem
The inspiratory flow rate determines the rate at which the ventilator delivers gas to the lungs. If the set respiratory rate is low, there is plenty of time for complete tidal volume to be delivered even if the inspiratory flow rate is low. However, if the respiratory rate is increased, then the time allowed for the ventilator to push gas into the lungs is reduced, and there may not be enough time for the complete volume to be delivered. The simple solution is to increase the inspiratory flow rate. By increasing the inspiratory flow rate, then the ventilator can still deliver the set tidal volume even though the time allotted to each inspiration has been reduced.

Pressure Limit Problem
During inspiration, the ventilator pushes gas into the lungs. As the volume of gas in the lungs rises, the pressure required to push the gas rises as well. Because excessive pressure can damage the lungs, the ventilator will stop delivering gas once the pressure exceeds a set limit. This“peak pressure limit” is an adjustable setting on the ventilator that is built into the anesthesia machine. Once the pressure measured by the ventilator reaches the set pressure limit, then gas delivery stops and the delivered tidal volume is only the amount of gas that was delivered before the pressure limit was reached. The problem we face is that the pressure that is measured by the ventilator as it pushes gas toward the lungs is not the same as the actual pressure in the lungs. The pressure that the ventilator sees is the pressure in the lungs plus all of the back pressure required to push gas through additional devices placed in the path between the ventilator and the lungs. These devices include the endotracheal tube, the bacterial/viral filter, ANEclear, the breathing circuit hose, the anesthesia machine check valve, etc. The amount of back pressure is small when the gas flow rate is low. This is often the case when the respiration rate is low. But when the gas flow rate is increased, the added back pressure caused by pushing gas rapidly through the breathing circuit rises. In some cases, doubling the inspiratory flow rate can raise the back pressure fourfold.
On some newer electronic ventilators, raising the respiration rate tells the ventilator to automatically raise the flow rate during inspiration. This means that when you double the respiration rate, you tell the ventilator to double the gas flow rate during inspiration. This causes the back pressure to rise causing the pressure to exceed the limit and therefore causing the delivered tidal volume to drop.
As an example, consider a situation in which the respiration rate is set at 10 breaths per minute during maintenance and the added back pressure during each inspiration is 8 cm H2O. If the breath rate is increased to 20 breaths per minute during emergence, then the back pressure might increase from 8 to 32 cm. H2O. Adding 32 cm H2O of back pressure to the actual pressure in the lungs of about 15 cm H2O will exceed a normal peak pressure limit set at 30 cm H2O and therefore only a small volume will be delivered to the lungs.
The simple solution to this problem is to simply raise the set peak pressure limit on the ventilator. This will allow the full tidal volume to be delivered regardless of the back pressure induced by increased flow rate. Note that on some machines, the high pressure limit is set by adjusting an alarm limit. This means that adjusting the high pressure alarm limit automatically adjusts the maximum pressure that the ventilator will deliver.
The peak inspiratory pressure limit is provided as a safety mechanism to prevent “barotraumas” or damage to the lungs due to over-inflation. Most clinicians understand that the actual pressure in the lungs is much less than the pressure seen by their ventilator and displayed on their monitor screens and that increasing the pressure limit does not mean that the lungs will experience the set pressure limit. However, there is a limit beyond which the pressure limit can not be increased.
If the pressure limit is already at the maximum safe level, an alternative approach is to increase the time allotted to inspiration during each breath by adjusting the I:E ratio setting on the ventilator. The I:E ratio is the ratio of inspiration time relative to expiration time for each breath. For example, if the I:E ratio is set at 1:3, then for every one second of inspiration time, there will be three seconds of expiration. Decreasing the I:E ratio gives more time for inspiration and therefore lowers the flow rate needed to deliver the set tidal volume. Lower flow rates mean less back pressure so more volume can be delivered to the lungs without reaching the peak pressure limit.
As an example, consider a case in which the set respiration rate is 10 breaths per minute and the I:E ratio is 1:3 during maintenance. This means that inspiration lasts 1.5 seconds and expiration lasts for 4.5 seconds for each breath. If the breath rate is doubled during emergence, then the time allowed for each inspiration drops to 0.75 seconds, and the ventilator would need to double the flow rate to deliver the entire breath in the shortened time. The doubled flow rate will cause an increase in back pressure causing the peak pressure limit to be reached and the tidal volume to be decreased. If the I:E ratio is adjusted lower, to 1:1, then the time allowed for inspiration remains at 1.5 seconds and the ventilator does not have to increase flow rate even though the respiration rate has doubled. In this manner, the respiratory rate can be doubled and the peak pressure does not increase.
Another method of raising the delivered volume is to increase the respiratory rate less dramatically. For example, doubling the respiration rate, without changing the I:E ratio might cause a fourfold increase in back pressure; however, a 50% increase in respiration rate might only raise the back pressure twofold. This means that if respiratory rate is high and tidal volume has fallen, it may be wise to decrease the respiration rate until the tidal volume has been restored to its set value. One strategy is to decrease the respiratory rate in small steps (1-2 breaths per minute) until the set tidal volume is delivered.
So the first strategy is to increase the peak pressure limit. If the pressure limit is already at the highest safe level, then adjust the I:E ratio down. Both of these adjustments can be done prior to emergence. If neither of these strategies is available, decrease respiration rate in steps of 1-2 breaths/minute until the set tidal volume is achieved.
MONITORING ISSUES
Two Tidal Volumes
Electronic anesthesia machines display two versions of tidal volume. One is the set tidal volume selected by the user; the other is measured tidal volume. The measured tidal volume is the volume of exhaled gas for the most recent breath. When there is a problem with the inspiratory flow rate or the pressure limit, the measured tidal volume will be less than the set volume.
Watch The Bellows
 If you cannot see, or cannot locate, the measured tidal volume display on the anesthesia machine screen, watch the bellows. The bellows rise and fall with each breath. There are marks on the side of the bellows showing the volume corresponding to the position of the bellows. If the rise and fall of the anesthesia machine bellows is not approximately equal to the set tidal volume, then the set tidal volume is not being delivered. If the movement of the bellows does not indicate at least 500 ml volume during emergence, ANEclear will not give the rapid emergence that is expected.
If you cannot see, or cannot locate, the measured tidal volume display on the anesthesia machine screen, watch the bellows. The bellows rise and fall with each breath. There are marks on the side of the bellows showing the volume corresponding to the position of the bellows. If the rise and fall of the anesthesia machine bellows is not approximately equal to the set tidal volume, then the set tidal volume is not being delivered. If the movement of the bellows does not indicate at least 500 ml volume during emergence, ANEclear will not give the rapid emergence that is expected.
Minute Volume Delay
Remember that “tidal volume” is the volume of gas delivered during each breath, “respiration rate” is the number of breaths delivered each minute and “minute volume” is the total volume of the breaths delivered in the past minute. Since the minute volume is the sum of breaths given in the past minute, it will not reflect changes in tidal volume and or respiration rate until nearly a minute later. That is why the displayed minute volume often does not equal tidal volume multiplied by respiration rate. This delay between when adjustments are made and when the displayed minute volume is correct can lead to errors in ventilator adjustment.
A DRY RUN
If safe and practical, hyperventilate the patient during the maintenance phase of the anesthetic. Test your strategy for 2-3 minutes during the time when there is not much for the anesthesiologist/ CRNA to do during the surgery. Remember that it will take at least 1 minute to observe the complete effect of any setting change on the displayed minute volume. In any case they can quickly see that the tidal volume does not change when respiration rate in increased. This will give them a chance to test their settings for pressure
limit, I:E ratio etc. and be sure that all is as it should be prior to emergence
DEMONSTRATION CASE
The photo below was taken at a demonstration at a University located in the south eastern area of the United States. The set tidal volume was 875 ml. and the measured tidal volume was much less, only 156 ml. The machine showed warning messages saying that the set tidal volume was not delivered and that the peak pressure was high, but neither were noticed. The displayed minute volume was 9.4 liters, while the actual, instantaneous minute volume was only 3.9 liters. The displayed minute volume is left over from the minute before emergence when the tidal volume was still large. The peak pressure was 42 cm H2O which was in excess of the pressure limit setting which was most likely set at 40 cm H2O. The I:E ratio was set at 1:2.
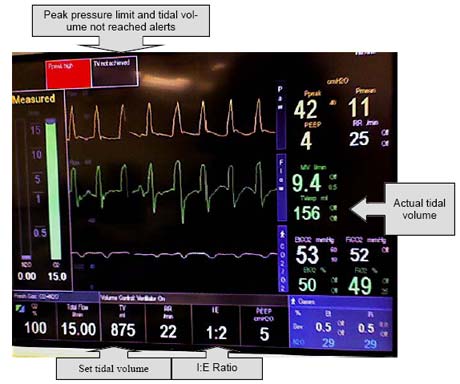
In this case, the emergence was slower than expected. The set tidal volume was large and the delivered tidal volume was sufficient prior to emergence when the respiratory rate was 11 breaths per minute. When the respiratory rate was increased to 22, the pressure limit was reached during inspiration and the tidal volume dropped. In this case, the minute volume during emergence was less than half the maintenance minute volume. Because the small tidal volume was about the same as the patient’s dead volume (volume in the trachea that does not participate in gas exchange) there was virtually no gas exchange in the lungs. Had this problem been recognized, any of the three strategies suggested earlier could have corrected this situation. Either raising the peak pressure limit, adjusting the I:E ratio to 1:1 or stepping down the respiration rate would have caused higher tidal volumes and a faster emergence.