Using ANEclear with a Laryngeal Mask Airway
Derek Sakata, MD – Professor (Clinical) of Anesthesiology, University of Utah
Summary
 ANEclear provides a safer and faster emergence from inhaled anesthetics in spontaneously breathing patients. It can be used during emergence when the patient is breathing through a Laryngeal Mask Airway (LMA), or a face mask. In spontaneously breathing patients, an activated ANEclear uses rebreathing of CO2 to raise the patient’s PaCO2. This respiratory stimulant increases the patient’s spontaneous tidal volume and respiratory rate, which speeds the rate of removal of the inhaled anesthetic from the lungs. The respiratory stimulant also helps the patient breathe through the laryngeal mask or face mask, the airway filter, ANEclear and the anesthesia circuit, overcoming their combined resistance. When ANEclear is used in spontaneously breathing patients, respiratory monitoring is needed to ensure that the patient breathes with a tidal volume of at least 500 mL. This provides adequate oxygenation during rebreathing. If the fraction of inspired oxygen drops below 35% or the oxygen saturation drops below 90%, ANEclear should be deactivated.
ANEclear provides a safer and faster emergence from inhaled anesthetics in spontaneously breathing patients. It can be used during emergence when the patient is breathing through a Laryngeal Mask Airway (LMA), or a face mask. In spontaneously breathing patients, an activated ANEclear uses rebreathing of CO2 to raise the patient’s PaCO2. This respiratory stimulant increases the patient’s spontaneous tidal volume and respiratory rate, which speeds the rate of removal of the inhaled anesthetic from the lungs. The respiratory stimulant also helps the patient breathe through the laryngeal mask or face mask, the airway filter, ANEclear and the anesthesia circuit, overcoming their combined resistance. When ANEclear is used in spontaneously breathing patients, respiratory monitoring is needed to ensure that the patient breathes with a tidal volume of at least 500 mL. This provides adequate oxygenation during rebreathing. If the fraction of inspired oxygen drops below 35% or the oxygen saturation drops below 90%, ANEclear should be deactivated.
The Laryngeal Mask Airway
The laryngeal mask airway (LMA) is a device that is used to help facilitate spontaneous respiration while under general anesthesia, Figure 1. While under general anesthesia with volatile or intravenous anesthetics, a patient’s airway anatomy may relax and breathing may be obstructed. The LMA is a less intrusive and therefore less irritating device than the endotracheal tube. The LMA keeps the airway open by providing a direct airway conduit to the trachea but does not extend into the trachea as does the endotracheal tube.
LMA Diagram
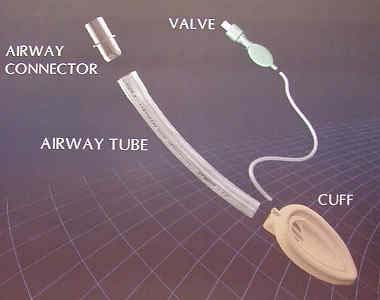
Figure 1
LMA Usage
The LMA may be chosen over the endotracheal tube because of its relative ease of placement, less irritability of the airway, less resistance for spontaneous breathing and therefore possibly smaller amount of anesthetic needed. Since the LMA may require less anesthetic and is not placed into the trachea, which is therefore less irritating, most anesthetists perceive that by using the LMA, patients may exit anesthesia faster. Since the LMA is considered a less adequate method to secure the airway, it will most likely only be used when the airway is more geographically accessible to the anesthetist.
LMA
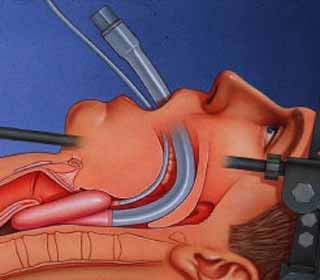
Figure 2.
It also does not protect the airway from gastric contents like an endotracheal tube. It is also not considered to be a device of choice for positive pressure ventilation for a prolonged period of time. Therefore, it will only be used in cases in which aspiration of gastric contents is of relatively low risk, shorter cases and overall less complex surgical cases.
ANEclear with the LMA
ANEclear has been used extensively with the LMA and has shown positive results. As stated above, during spontaneous ventilation at emergence, ANEclear may be activated to facilitate emergence from a general anesthetic maintained with a volatile agent. ANEclear functions well in facilitating rebreathing of CO2 with the LMA. This will then steadily allow the patient to increase his or her minute ventilation in response to the rise in CO2. This increased respiration will actively reverse the volatile anesthetic.
ANEclear, LMA and Oxygenation
It must be emphasized again that tidal volumes of 500 mL are recommended in order to maintain adequate oxygenation while using ANEclear at its maximum dead space of 750 mL. If tidal volumes are less than 500 mL, as stated above, the anesthetist must pay careful attention to the FiO2 and oxygen saturation. Again, remember that the patient will most likely increase his or her tidal volume and or respiratory rate in response to the increasing CO2.
ANEclear, LMA and Expectations
ANEclear will help facilitate emergence of patients from volatile anesthetics while using the LMA. It is important to realize that emergence will be dependent on the amount of minute ventilation a patient is taking. This may or may not be a lot depending on factors for spontaneous ventilation as stated above. It is also important to remember that the LMA is not as stimulating as the endotracheal tube. Therefore, the emergence with an LMA most likely will be smoother than that with an endotracheal tube, but possibly not quite as rapid.
ENSURING SAFE SPONTANEOUS VENTILATION
Oxygenation
The primary safe endpoint is that the patient maintains a tidal volume that allows for adequate oxygenation. Again, a safe tidal volume to be used in conjunction with an activated ANEclear is at least 500 mL. If tidal volumes are less than 500 mL, special attention should be paid to both the fraction of inspired oxygen and oxygen saturation. If the fraction of inspired oxygen drops below 35% or the oxygen saturation drops to less than or equal to 90%, ANEclear should be deactivated. Without the re-breathing dead space, it may be possible that the patient may decrease his or her minute ventilation as the carbon dioxide is “blown-off.”
Nitrous Oxide Removal
If nitrous oxide is used during the case and not discontinued well before the end of the case, it may be possible for the patient to continue to rebreathe the nitrous oxide and not rapidly emerge from anesthesia. This condition may be apparent if one were to see the fraction of inspired nitrous oxide not appreciably drop on successive breaths. It should be noted that even if the fraction of inspired oxygen and oxygen saturation remains within a safe range, it may be prudent to deactivate ANEclear after the end tidal volatile agent concentration reaches less than or equal to one-third of its MAC value. Again, expect that the minute ventilation may decrease.
Coughing on the Endotracheal Tube
If coughing due to tracheal irritation occurs, aside from being really difficult to watch, the tidal volume may suffer. In addition, since the patient is more stimulated, oxygen consumption and CO2 production may increase. As stated above, this situation is more apt to occur in patients who are smokers or are asthmatics. It is also more apt to occur in patients who are being control ventilated. Bronchospasm, or closing of the small airways in the lungs, is more apt to occur during these coughing fits. In addition, these patients may be in stage II and are more apt to experience laryngospasm, closing of the vocal cords or airway, if the endotracheal tube is pulled too early. In this situation, it would probably be advisable to deactivate ANEclear and allow the clinician to proceed as he or she would normally. This type of emergence may occur with or without ANEclear device.
ANEclear / LMA CASE STUDIES
Case Study #1
53 year old, 75 kg, Caucasian male with history of hypertension scheduled for ORIF of left tibial plateau fracture. The patient received premedication with midazolam 2 mgs.
Induction
The patient was taken to the operating room. Monitors were placed. Preoxygenation occurred. The patient was induced for a general anesthetic with:
- Fentanyl 50 mcgs
- Lidocaine 80 mgs
- Propofol 200 mgs
After loss of consciousness, a LMA #5 was placed without difficulty.
Maintenance
The patient was maintained with 2.0% sevoflurane. Surgery commenced. 600 mcgs of fentanyl were titrated throughout the case. There were no difficulties and the surgery ended 3 hours later. Right before emergence, the patient was breathing at tidal volumes equal to 600 mL at 9 times per minute. His end tidal carbon dioxide was 51 mmHg.
Emergence
ANEclear was activated. The patient immediately began to re-breathe carbon dioxide. The inspired anesthetic agent went to zero within 5-6 breaths. The patient progressively began to increase both his tidal volume and respiratory rate to prevent his end tidal carbon dioxide from going above 51 mmHg. His tidal volume went to 1100 mL at 18 breaths per minute. The patient was awake and had the LMA removed after 3.5 minutes. His minute ventilation right before removal of the LMA was approximately 20 liters per minute.
Case Study #2
42 year old 65 kg Hispanic female, otherwise healthy scheduled for ORIF of right distal radial fracture. The patient received premedication with midazolam 2 mgs.
Induction
The patient was taken to the operating room. Monitors were placed. Preoxygenation occurred. The patient was induced for a general anesthetic with:
- Fentanyl 50 mcgs
- Lidocaine 60 mgs
- Propofol 170 mgs
After loss of consciousness, a LMA #4 was placed without difficulty.
Maintenance
The patient was maintained with 2.0% sevoflurane. Surgery commenced. 500 mcgs of fentanyl were titrated throughout the case. There were no difficulties and the surgery ended 2 hours later. Right before emergence, the patient was breathing at tidal volumes equal to 450-500 mL at 6 times per minute. Her end tidal carbon dioxide was 47 mmHg.
Emergence
ANEclear was activated. The patient immediately began to re-breathe carbon dioxide. The inspired anesthetic agent went to zero within 5-6 breaths. The patient progressively began to increase both her tidal volume and respiratory rate. The tidal volume achieved 600 mL and rate 12 breaths per minute. The end tidal CO2 rose to 60 mmHg. The patient was awake and had the LMA removed after 6.0 minutes. Her minute ventilation right before removal of the LMA was approximately 8 liters per minute.
Using ANEclear with a Laryngeal Mask Airway
Derek Sakata, MD – Professor (Clinical) of Anesthesiology, University of Utah
Summary

ANEclear provides a safer and faster emergence from inhaled anesthetics in spontaneously breathing patients. It can be used during emergence when the patient is breathing through a Laryngeal Mask Airway (LMA), or a face mask. In spontaneously breathing patients, an activated ANEclear uses rebreathing of CO2 to raise the patient’s PaCO2. This respiratory stimulant increases the patient’s spontaneous tidal volume and respiratory rate, which speeds the rate of removal of the inhaled anesthetic from the lungs. The respiratory stimulant also helps the patient breathe through the laryngeal mask or face mask, the airway filter, ANEclear and the anesthesia circuit, overcoming their combined resistance. When ANEclear is used in spontaneously breathing patients, respiratory monitoring is needed to ensure that the patient breathes with a tidal volume of at least 500 mL. This provides adequate oxygenation during rebreathing. If the fraction of inspired oxygen drops below 35% or the oxygen saturation drops below 90%, ANEclear should be deactivated.
The Laryngeal Mask Airway
The laryngeal mask airway (LMA) is a device that is used to help facilitate spontaneous respiration while under general anesthesia, Figure 1. While under general anesthesia with volatile or intravenous anesthetics, a patient’s airway anatomy may relax and breathing may be obstructed. The LMA is a less intrusive and therefore less irritating device than the endotracheal tube. The LMA keeps the airway open by providing a direct airway conduit to the trachea but does not extend into the trachea as does the endotracheal tube.
LMA Diagram
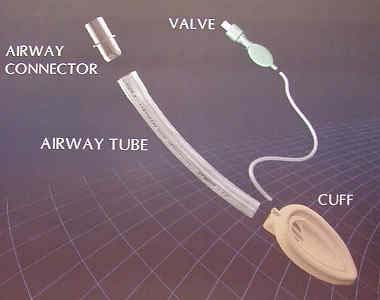
Figure 1
LMA Usage
The LMA may be chosen over the endotracheal tube because of its relative ease of placement, less irritability of the airway, less resistance for spontaneous breathing and therefore possibly smaller amount of anesthetic needed. Since the LMA may require less anesthetic and is not placed into the trachea, which is therefore less irritating, most anesthetists perceive that by using the LMA, patients may exit anesthesia faster. Since the LMA is considered a less adequate method to secure the airway, it will most likely only be used when the airway is more geographically accessible to the anesthetist.
LMA
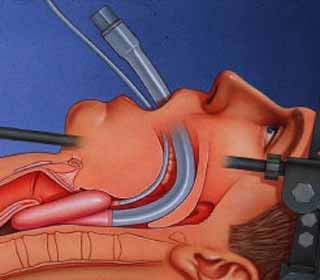
Figure 2.
It also does not protect the airway from gastric contents like an endotracheal tube. It is also not considered to be a device of choice for positive pressure ventilation for a prolonged period of time. Therefore, it will only be used in cases in which aspiration of gastric contents is of relatively low risk, shorter cases and overall less complex surgical cases.
ANEclear with the LMA
ANEclear has been used extensively with the LMA and has shown positive results. As stated above, during spontaneous ventilation at emergence, ANEclear may be activated to facilitate emergence from a general anesthetic maintained with a volatile agent. ANEclear functions well in facilitating rebreathing of CO2 with the LMA. This will then steadily allow the patient to increase his or her minute ventilation in response to the rise in CO2. This increased respiration will actively reverse the volatile anesthetic.
ANEclear, LMA and Oxygenation
It must be emphasized again that tidal volumes of 500 mL are recommended in order to maintain adequate oxygenation while using ANEclear at its maximum dead space of 750 mL. If tidal volumes are less than 500 mL, as stated above, the anesthetist must pay careful attention to the FiO2 and oxygen saturation. Again, remember that the patient will most likely increase his or her tidal volume and or respiratory rate in response to the increasing CO2.
ANEclear, LMA and Expectations
ANEclear will help facilitate emergence of patients from volatile anesthetics while using the LMA. It is important to realize that emergence will be dependent on the amount of minute ventilation a patient is taking. This may or may not be a lot depending on factors for spontaneous ventilation as stated above. It is also important to remember that the LMA is not as stimulating as the endotracheal tube. Therefore, the emergence with an LMA most likely will be smoother than that with an endotracheal tube, but possibly not quite as rapid.
ENSURING SAFE SPONTANEOUS VENTILATION
Oxygenation
The primary safe endpoint is that the patient maintains a tidal volume that allows for adequate oxygenation. Again, a safe tidal volume to be used in conjunction with an activated ANEclear is at least 500 mL. If tidal volumes are less than 500 mL, special attention should be paid to both the fraction of inspired oxygen and oxygen saturation. If the fraction of inspired oxygen drops below 35% or the oxygen saturation drops to less than or equal to 90%, ANEclear should be deactivated. Without the re-breathing dead space, it may be possible that the patient may decrease his or her minute ventilation as the carbon dioxide is “blown-off.”
Nitrous Oxide Removal
If nitrous oxide is used during the case and not discontinued well before the end of the case, it may be possible for the patient to continue to rebreathe the nitrous oxide and not rapidly emerge from anesthesia. This condition may be apparent if one were to see the fraction of inspired nitrous oxide not appreciably drop on successive breaths. It should be noted that even if the fraction of inspired oxygen and oxygen saturation remains within a safe range, it may be prudent to deactivate ANEclear after the end tidal volatile agent concentration reaches less than or equal to one-third of its MAC value. Again, expect that the minute ventilation may decrease.
Coughing on the Endotracheal Tube
If coughing due to tracheal irritation occurs, aside from being really difficult to watch, the tidal volume may suffer. In addition, since the patient is more stimulated, oxygen consumption and CO2 production may increase. As stated above, this situation is more apt to occur in patients who are smokers or are asthmatics. It is also more apt to occur in patients who are being control ventilated. Bronchospasm, or closing of the small airways in the lungs, is more apt to occur during these coughing fits. In addition, these patients may be in stage II and are more apt to experience laryngospasm, closing of the vocal cords or airway, if the endotracheal tube is pulled too early. In this situation, it would probably be advisable to deactivate ANEclear and allow the clinician to proceed as he or she would normally. This type of emergence may occur with or without ANEclear device.
ANEclear / LMA CASE STUDIES
Case Study #1
53 year old, 75 kg, Caucasian male with history of hypertension scheduled for ORIF of left tibial plateau fracture. The patient received premedication with midazolam 2 mgs.
Induction
The patient was taken to the operating room. Monitors were placed. Preoxygenation occurred. The patient was induced for a general anesthetic with:
- Fentanyl 50 mcgs
- Lidocaine 80 mgs
- Propofol 200 mgs
After loss of consciousness, a LMA #5 was placed without difficulty.
Maintenance
The patient was maintained with 2.0% sevoflurane. Surgery commenced. 600 mcgs of fentanyl were titrated throughout the case. There were no difficulties and the surgery ended 3 hours later. Right before emergence, the patient was breathing at tidal volumes equal to 600 mL at 9 times per minute. His end tidal carbon dioxide was 51 mmHg.
Emergence
ANEclear was activated. The patient immediately began to re-breathe carbon dioxide. The inspired anesthetic agent went to zero within 5-6 breaths. The patient progressively began to increase both his tidal volume and respiratory rate to prevent his end tidal carbon dioxide from going above 51 mmHg. His tidal volume went to 1100 mL at 18 breaths per minute. The patient was awake and had the LMA removed after 3.5 minutes. His minute ventilation right before removal of the LMA was approximately 20 liters per minute.
Case Study #2
42 year old 65 kg Hispanic female, otherwise healthy scheduled for ORIF of right distal radial fracture. The patient received premedication with midazolam 2 mgs.
Induction
The patient was taken to the operating room. Monitors were placed. Preoxygenation occurred. The patient was induced for a general anesthetic with:
- Fentanyl 50 mcgs
- Lidocaine 60 mgs
- Propofol 170 mgs
After loss of consciousness, a LMA #4 was placed without difficulty.
Maintenance
The patient was maintained with 2.0% sevoflurane. Surgery commenced. 500 mcgs of fentanyl were titrated throughout the case. There were no difficulties and the surgery ended 2 hours later. Right before emergence, the patient was breathing at tidal volumes equal to 450-500 mL at 6 times per minute. Her end tidal carbon dioxide was 47 mmHg.
Emergence
ANEclear was activated. The patient immediately began to re-breathe carbon dioxide. The inspired anesthetic agent went to zero within 5-6 breaths. The patient progressively began to increase both her tidal volume and respiratory rate. The tidal volume achieved 600 mL and rate 12 breaths per minute. The end tidal CO2 rose to 60 mmHg. The patient was awake and had the LMA removed after 6.0 minutes. Her minute ventilation right before removal of the LMA was approximately 8 liters per minute.