ANEclear with Spontaneously Breathing Patients
Derek Sakata, MD – Professor (Clinical) of Anesthesiology, University of Utah
 Summary
Summary
ANEclear provides for a safer and faster emergence from inhaled anesthetics in spontaneously breathing patients. During emergence in your spontaneously breathing patients, an activated ANEclear utilizes partial rebreathing of carbon dioxide to raise the partial pressure of carbon dioxide in blood. This respiratory stimulant increases the patient’s spontaneous tidal volume and respiratory rate, which accelerates the clearance of the inhaled anesthetic from the lungs.
This same respiratory stimulant in arterial blood (PaCO2) will also increase cerebral blood flow Figure 1., brain washout, and activation of neurons that control the spontaneous drive to breathe. This is especially important during spontaneous ventilation, while under the influence of inhaled anesthetics and opioids due to their respiratory depressing effects. The amount of increase in minute ventilation is unknown given patient variability and the amount, as well as the type of medications used that might cause respiratory depression such as; opioids, benzodizapines, nitrous oxide and neuromuscular blockade agents.
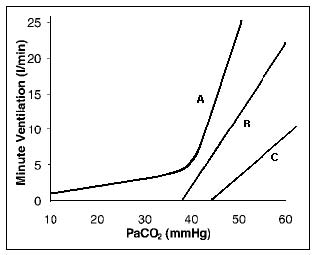
Figure 1
ANEclear and Spontaneously Breathing Patients
ANEclear adds 1.8 cm H20 at 30 L/min of airway resistance into the breathing circuit. This added resistance does increase the work of breathing for a spontaneously breathing patient as ANEclear is typically a very small percentage of the total circuit resistance. This added resistance is comparable to adding an additional large-diameter bacterial filter into the breathing circuit.
Emphasis on maintaining adequate delivered tidal volume of at least 500 mLs is vital in the safety and efficacy of ANEclear especially in spontaneously breathing patients. This tidal volume level will provide adequate oxygenation during rebreathing. If tidal volumes are less than 500 mL with the rebreathing loop fully extended, it may be possible to continue the use of ANEclear if the patient tolerates tidal volumes less than 500 mLs, however special attentiveness should be paid to both the fraction of inspired oxygen and oxygen saturation. If FIO2 drops below 35% or oxygen saturation drops below 90% ANEclear should be deactivated.
In order to obtain maximum benefit from ANEclear in a spontaneously breathing patient it may be desirable to augment their tidal volume by bagging or using your ventilator in pressure support mode if available, as these methods will increase and optimize minute ventilation. The work of breathing can be reduced in a spontaneously breathing patient by the use of Pressure Support Ventilation (PSV) or Synchronous Intermittent Mandatory Ventilation (SIMV), if these are available on your anesthesia machine. Pressure Support when maintenance tidal volumes are already greater than 500 mLs may increase tidal volumes well above 750 mLs and may cause over-breathing of ANEclear’s dead space and loss of carbon dioxide out of the rebreathing loop back into the anesthesia circuit for scavenging, ultimately decreasing the effectiveness of ANEclear on cerebral washout and reversal of the volatile anesthetic.
Patients in which minute ventilation is disrupted by excessive coughing could also benefit from synchronous intermittent mandatory ventilation to augment baseline ventilation while supporting spontaneous attempts. Additionally, LMAs in spontaneously breathing patients are less stimulating and can cause less coughing. Therefore, LMAs usually provide for the best environment for maximal ventilation and removal of inhaled anesthetic in a spontaneously breathing patient. Ensure the patient’s minute ventilation remains intact when discontinuing SIMV or PSV before removal of the LMA.
In spontaneously breathing patients where maintenance end-tidal carbon dioxide levels are above 45 mmHG prior to emergence, activate ANEclear with the rebreathing loop contracted. This will minimize the dead space of ANEclear to 400 mLs and allow the clinician to control the amount of partial rebreathing and best manage the extent of hypercapnia. The rebreathing loop can slowly be expanded to increase the amount of rebreathing and levels of carbon dioxide, when it has been determined that higher carbon dioxide levels can be tolerated.
Use a bite block. In vigorous, spontaneous ventilation biting on the endotracheal tube or LMA could greatly increase the chance of a patient experiencing negative pressure pulmonary edema.
Discontinuing ANEclear before the patient is completely awake can slow recovery. Monitor your patient for the classic signs of emergence from inhaled anesthesia and extubate based on your best clinical judgment.
ANEclear with Spontaneously Breathing Patients
Derek Sakata, MD, Assistant Professor of Anesthesiology University of Utah Department of Anesthesiology
 Summary
Summary
ANEclear provides for a safer and faster emergence from inhaled anesthetics in spontaneously breathing patients. During emergence in your spontaneously breathing patients, an activated ANEclear utilizes partial rebreathing of carbon dioxide to raise the partial pressure of carbon dioxide in blood. This respiratory stimulant increases the patient’s spontaneous tidal volume and respiratory rate, which accelerates the clearance of the inhaled anesthetic from the lungs.
This same respiratory stimulant in arterial blood (PaCO2) will also increase cerebral blood flow Figure 1., brain washout, and activation of neurons that control the spontaneous drive to breathe. This is especially important during spontaneous ventilation, while under the influence of inhaled anesthetics and opioids due to their respiratory depressing effects. The amount of increase in minute ventilation is unknown given patient variability and the amount, as well as the type of medications used that might cause respiratory depression such as; opioids, benzodizapines, nitrous oxide and neuromuscular blockade agents.
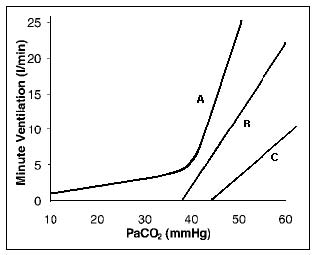
Figure 1
ANEclear and Spontaneously Breathing Patients
ANEclear adds 1.8 cm H20 at 30 L/min of airway resistance into the breathing circuit. This added resistance does increase the work of breathing for a spontaneously breathing patient as ANEclear is typically a very small percentage of the total circuit resistance. This added resistance is comparable to adding an additional large-diameter bacterial filter into the breathing circuit.
Emphasis on maintaining adequate delivered tidal volume of at least 500 mLs is vital in the safety and efficacy of ANEclear especially in spontaneously breathing patients. This tidal volume level will provide adequate oxygenation during rebreathing. If tidal volumes are less than 500 mL with the rebreathing loop fully extended, it may be possible to continue the use of ANEclear if the patient tolerates tidal volumes less than 500 mLs, however special attentiveness should be paid to both the fraction of inspired oxygen and oxygen saturation. If FIO2 drops below 35% or oxygen saturation drops below 90% ANEclear should be deactivated.
In order to obtain maximum benefit from ANEclear in a spontaneously breathing patient it may be desirable to augment their tidal volume by bagging or using your ventilator in pressure support mode if available, as these methods will increase and optimize minute ventilation. The work of breathing can be reduced in a spontaneously breathing patient by the use of Pressure Support Ventilation (PSV) or Synchronous Intermittent Mandatory Ventilation (SIMV), if these are available on your anesthesia machine. Pressure Support when maintenance tidal volumes are already greater than 500 mLs may increase tidal volumes well above 750 mLs and may cause over-breathing of ANEclear’s dead space and loss of carbon dioxide out of the rebreathing loop back into the anesthesia circuit for scavenging, ultimately decreasing the effectiveness of ANEclear on cerebral washout and reversal of the volatile anesthetic.
Patients in which minute ventilation is disrupted by excessive coughing could also benefit from synchronous intermittent mandatory ventilation to augment baseline ventilation while supporting spontaneous attempts. Additionally, LMAs in spontaneously breathing patients are less stimulating and can cause less coughing. Therefore, LMAs usually provide for the best environment for maximal ventilation and removal of inhaled anesthetic in a spontaneously breathing patient. Ensure the patient’s minute ventilation remains intact when discontinuing SIMV or PSV before removal of the LMA.
In spontaneously breathing patients where maintenance end-tidal carbon dioxide levels are above 45 mmHG prior to emergence, activate ANEclear with the rebreathing loop contracted. This will minimize the dead space of ANEclear to 400 mLs and allow the clinician to control the amount of partial rebreathing and best manage the extent of hypercapnia. The rebreathing loop can slowly be expanded to increase the amount of rebreathing and levels of carbon dioxide, when it has been determined that higher carbon dioxide levels can be tolerated.
Use a bite block. In vigorous, spontaneous ventilation biting on the endotracheal tube or LMA could greatly increase the chance of a patient experiencing negative pressure pulmonary edema.
Discontinuing ANEclear before the patient is completely awake can slow recovery. Monitor your patient for the classic signs of emergence from inhaled anesthesia and extubate based on your best clinical judgment.