ANEclear Overview
 ANEclear is a patented disposable device technology to reverse the effects of inhaled volatile anesthetics in the brain at the end of surgery to return brain function, increase airway control and respiration, and improve patient alertness and orientation.
ANEclear is a patented disposable device technology to reverse the effects of inhaled volatile anesthetics in the brain at the end of surgery to return brain function, increase airway control and respiration, and improve patient alertness and orientation.
When general anesthesia is administered, anesthetics in the form of vapors are delivered to a patient. As the patient inhales the anesthetic vapor, the vapor enters the lungs, moves into the bloodstream and is carried by the blood to the brain. Inhaled anesthetics inhibit neurons in the brain, which play an essential role in brain functions including wakefulness and breathing.
Less than 5% of volatile anesthetics are metabolized, therefore once the surgical procedure has been completed, these unwanted residual anesthetics must be reversed in the brain and the molecules transported from the brain via the blood to the lungs in order to be transported out of the body.
Anesthesia providers typically taper off the anesthetic gases at the end of surgery and then wait for the effects to wear off. The effects of residual volatile anesthetics at the end of surgery include respiratory depression, delirium / cognitive dysfunction, and postoperative nausea and vomiting.
In addition to tapering off the anesthetic at the end of surgery, anesthesia providers may also increase ventilation to quickly remove the anesthetic gas from the lungs, but the resulting reduction of carbon dioxide (CO2) in the blood lowers cerebral blood flow and slows reversal of the agent in the brain, which delays brain function and wakefulness, and it decreases the respiratory drive resulting in delayed emergence and recovery. Hypoventilating patients will allow the CO2 to increase, however in the absence of increased ventilation concurrent with the increase in CO2, volatile anesthetics are not reversed in the neurons of the brain, and this process leaves the anesthetic gases in the lungs to return to the brain.
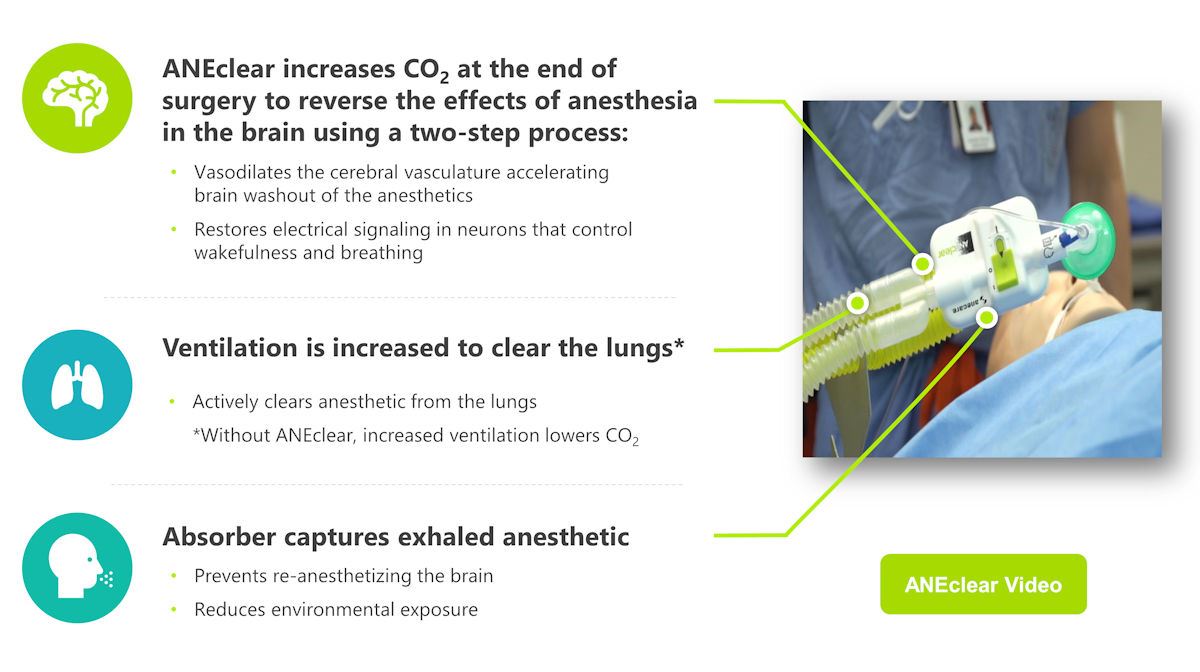
ANEclear fits between the patient and the Y-connector of the anesthesia breathing circuit. It can be installed at the beginning of the surgical case, or at the time of emergence. The device allows the anesthesia provider to increase the patient’s CO2, which thereby increases the partial pressure of arterial carbon dioxide (PaCO2), while simultaneously increasing ventilation. Increased PaCO2 has the effect of vasodilating the cerebral vasculature to accelerate brain washout of the anesthetics, and restoring neuron electrical signaling and brain function. Increased ventilation increases the diffusion gradient and transports the volatile anesthetic out of the body via the lungs. The device also includes an absorber to prevent patients from rebreathing their own exhaled volatile anesthetic.
ANEclear Overview
 ANEclear is a patented disposable device technology to reverse the effects of inhaled volatile anesthetics in the brain at the end of surgery to return brain function, increase airway control and respiration, and improve patient alertness and orientation.
ANEclear is a patented disposable device technology to reverse the effects of inhaled volatile anesthetics in the brain at the end of surgery to return brain function, increase airway control and respiration, and improve patient alertness and orientation.
When general anesthesia is administered, anesthetics in the form of vapors are delivered to a patient. As the patient inhales the anesthetic vapor, the vapor enters the lungs, moves into the bloodstream and is carried by the blood to the brain. Inhaled anesthetics inhibit neurons in the brain, which play an essential role in brain functions including wakefulness and breathing.
Less than 5% of volatile anesthetics are metabolized, therefore once the surgical procedure has been completed, these unwanted residual anesthetics must be reversed in the brain and the molecules transported from the brain via the blood to the lungs in order to be transported out of the body.
Anesthesia providers typically taper off the anesthetic gases at the end of surgery and then wait for the effects to wear off. The effects of residual volatile anesthetics at the end of surgery include respiratory depression, delirium / cognitive dysfunction, and postoperative nausea and vomiting.
In addition to tapering off the anesthetic at the end of surgery, anesthesia providers may also increase ventilation to quickly remove the anesthetic gas from the lungs, but the resulting reduction of carbon dioxide (CO2) in the blood lowers cerebral blood flow and slows reversal of the agent in the brain, which delays brain function and wakefulness, and it decreases the respiratory drive resulting in delayed emergence and recovery. Hypoventilating patients will allow the CO2 to increase, however in the absence of increased ventilation concurrent with the increase in CO2, volatile anesthetics are not reversed in the neurons of the brain, and this process leaves the anesthetic gases in the lungs to return to the brain.
ANEclear fits between the patient and the Y-connector of the anesthesia breathing circuit. It can be installed at the beginning of the surgical case, or at the time of emergence. The device allows the anesthesia provider to increase the patient’s CO2, which thereby increases the partial pressure of arterial carbon dioxide (PaCO2), while simultaneously increasing ventilation. Increased PaCO2 has the effect of vasodilating the cerebral vasculature to accelerate brain washout of the anesthetics, and restoring neuron electrical signaling and brain function. Increased ventilation increases the diffusion gradient and transports the volatile anesthetic out of the body via the lungs. The device also includes an absorber to prevent patients from rebreathing their own exhaled volatile anesthetic.
Clinical Benefits
- Accelerates washout of anesthetics from the brain
- Activates brain function to quickly restore the patient’s spontaneous drive to breathe
- Quickly orients patients and returns them to baseline
- Reduces the risk of agitation and delirium
- Helps patients remain awake and in control of their airway in the recovery unit
Economic Benefits
- Shortens early recovery in the OR by 52-64% (5-11 minutes)
- Reduces the risk of delirium and airway complications in the recovery unit
- Reduces the time to meet discharge criteria by up to 26% (23 minutes)